From Active-Duty Medical Officer To Gastroenterologist: A Conversation With Dr. Paredes
We caught up with Dr. Paredes to learn more about his work as a gastroenterologist, the biggest misconceptions around Crohn’s disease, and his hopes...

Find out how much Remicade infusions cost (with & without insurance) and how patients can lower costs.
Remicade is the brand name for a monoclonal biologic antibody (infliximab) used to treat several autoimmune diseases, including Crohn’s disease, ulcerative colitis, rheumatoid arthritis (in combination with methotrexate), Ankylosing spondylitis, psoriatic arthritis, and plaque psoriasis.
It works by inhibiting the action of a protein produced by the immune system known as tumor necrosis factor-alpha (TNF-alpha), which causes the immune system to attack healthy parts of the body. Those suffering from certain diseases may have too much TNF-alpha.
As with any FDA-approved IV treatment, Remicade can be expensive for a few reasons. First and foremost, it’s a prescription medication that’s expensive to produce. But most eligible patients also need regular infusions over long periods of time, which can contribute to higher costs.
Below, we break down how much Remicade infusions cost (with and without insurance), along with how patients can lower the cost of their infusions.
How much does Remicade cost?
The cost of Remicade can range between $3k-$12k per treatment, totaling upwards of $50k-150k per year.
How does insurance coverage impact the cost of Remicade?
How much the patient pays (aka out-of-pocket costs) is ultimately a function of the insurance plan. Every plan is different, but there are a few concepts that are important to remember:
Because of the high cost of Remicade infusion therapy, a patient will generally meet their deductible in the first infusion of the year, thus he/she would have limited out-of-pocket expenses for treatment costs the rest of the calendar year.
Don’t have insurance or aren’t in-network with your infusion center? It may be possible to bill your insurance company for the medication costs out-of-network. If out-of-network benefits aren’t available, you may be able to be seen as a Self Pay patient.
READ MORE: Prior Authorization: What It Is & How Long It Takes
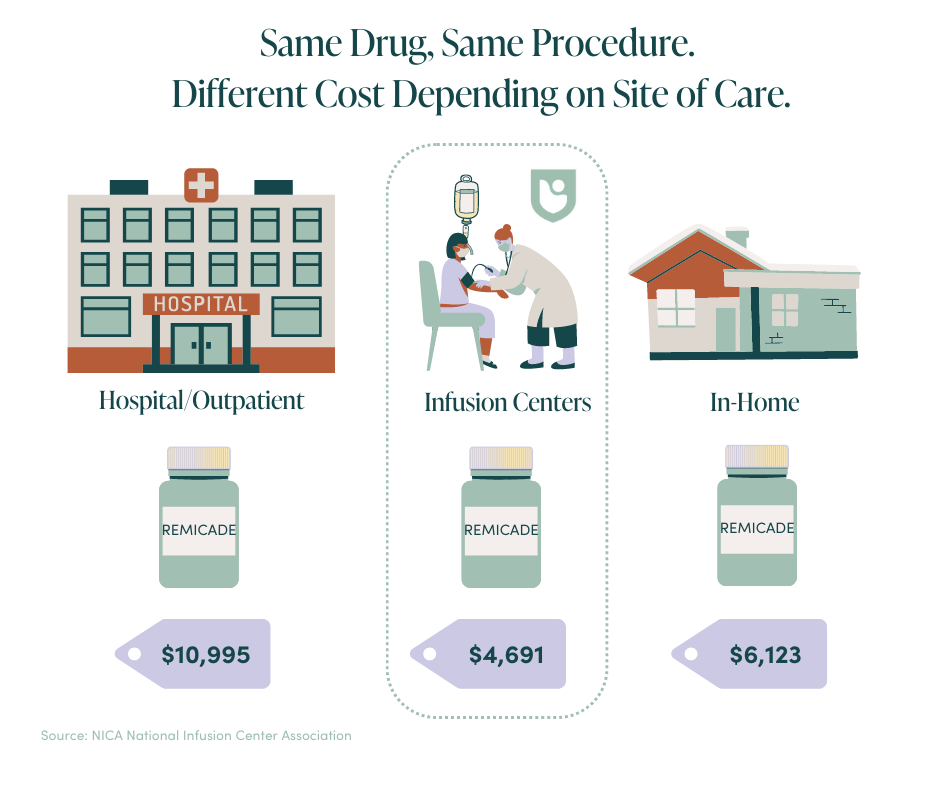
How does site of care impact the cost of Remicade?
The only decision a patient can make to influence the cost of their infusion is to decide where to receive treatment. Generally, there are three options where a patient may receive prescription drug infusion therapy from a healthcare professional:
Hospital outpatient is where 50-60% of infusions take place nationally. The cost is generally ~2x what it costs in the home or office. Home infusion has received a lot of press recently, but according to the National Infusion Center Association, it tends to be 50% more expensive than a healthcare provider’s office. The office setting will be the most affordable care setting for patients who have received a referral from their physician for infusion therapy.
READ MORE: How Much Does Infusion Therapy Cost?
How can I lower the cost of Remicade infusions?
Manufacturers have copay assistance and financial assistance programs to help offset the cost to patients, such as the Janssen Carepath Savings Program. Based on eligibility requirements, these programs may cover up to $20,000 per year per patient and significantly reduce, or remove, any financial burden a patient may face for the drug’s administration.
Interested in learning more about Remicade IV infusion (including side effects/allergic reactions, FAQs, enrollment qualifications, and more)? Here’s a full guide on what to expect, how long it takes to work, and a run-down of the differences between Remicade and its similar biologic drug/TNF blocker, Inflectra.
We caught up with Dr. Paredes to learn more about his work as a gastroenterologist, the biggest misconceptions around Crohn’s disease, and his hopes...
Learn more about Pemgarda, a groundbreaking preventative treatment offering the immunocompromised a new layer of defense against Covid-19.
Insurance, claims, prior authorization, precertification, deductibles….the list of healthcare terms goes on and on (and on). Needless to say, it’s...