From Active-Duty Medical Officer To Gastroenterologist: A Conversation With Dr. Paredes
We caught up with Dr. Paredes to learn more about his work as a gastroenterologist, the biggest misconceptions around Crohn’s disease, and his hopes...

One of the first questions we get from patients, healthcare leaders, and employers is… “how much does infusion therapy cost?”
Well, the answer is, it depends. There are a number of factors: the drug dose and frequency, insurance, the site of care. It can be quite overwhelming.
One thing is clear: FDA-approved IV treatment is expensive. It is expensive first and foremost because these drugs are expensive to produce. And they wouldn’t be covered by insurance if they weren’t highly effective. Most patients also need regular infusions over long periods of time. Treatment duration contributes to the overall cost as well.
Infusion costs can vary widely depending on drug and frequency
Considering the type of drug
The cost of infusion therapy depends largely on the therapy. Certain drugs, like Tepezza, can cost upwards of $16k per treatment (over $150k per course of treatment), while Remicade can range between $3k-$12k per treatment, totaling upwards of $50k-150k per year.
Considering the frequency of administration
The frequency is a function of the drug’s approved frequency and clinician orders. Patients on IV therapy receive treatment on average 6x per year for ongoing maintenance treatment.
Considering manufacturing costs
The drugs are expensive, primarily because they are so complicated to manufacture. Pharmaceutical companies invest billions of dollars in R&D for these drugs. Specialty drugs are biologic drugs with incredibly complex manufacturing processing, and, unlike traditional oral pills, specialty drugs have specialized shipping and storage requirements. All of these factors impact the ultimate cost paid by patients and health plans.
Insurance impacts what the patient actually pays
How much the patient pays (aka out-of-pocket costs) is ultimately a function of the patient’s insurance coverage. Every plan is different, but there are a few concepts that a patient should remember:
Because of the high cost of infusion therapy, a patient will generally meet their deductible in the first infusion of the year, thus he/she would have limited out-of-pocket expenses for treatment costs the rest of the year.
Site of care has a large impact on cost
The only decision a patient can make to influence the cost of their infusion is to decide where to receive treatment. Generally, there are three options where a patient may receive infusion therapy.
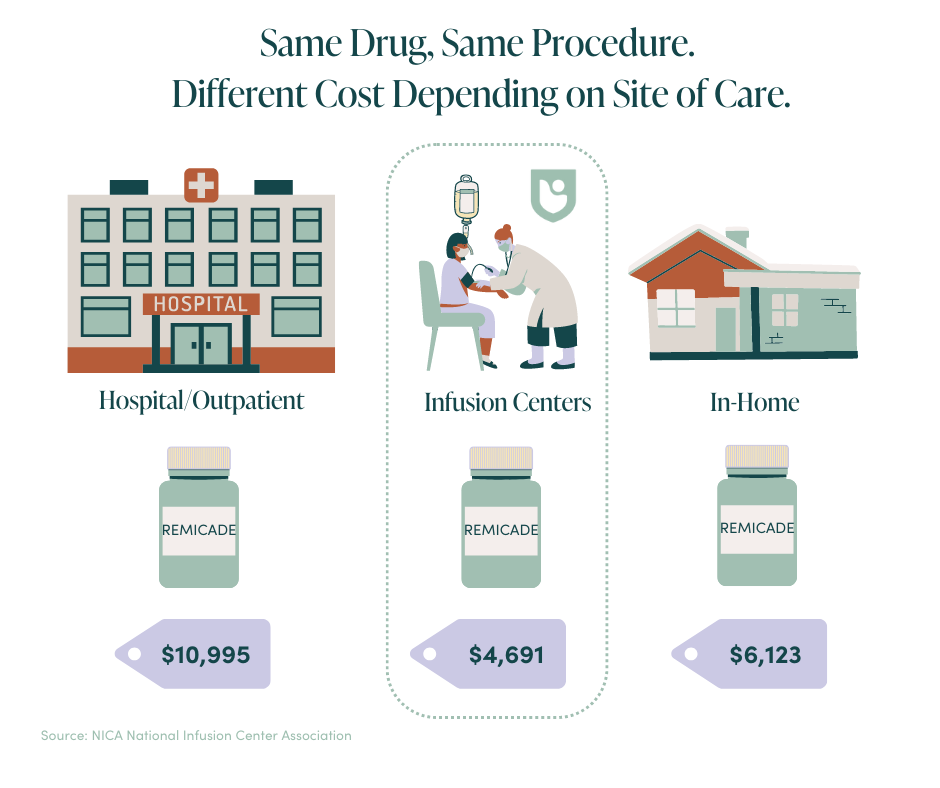
Hospital outpatient is where 50-60% of infusions take place nationally. The cost is generally ~2x what it costs in the home or office. Home infusion has received a lot of press recently, but according to the National Infusion Center Association, it tends to be 50% more expensive than a healthcare provider’s office. The office setting will be the most affordable care setting for patients who have received a referral from their physician for infusion therapy.
So you were prescribed infusion therapy?
We have spent much of this article describing how and why infusion therapy is expensive and some factors impacting cost. Infusion therapy is expensive and this can be overwhelming and make patients question the decision to receive infusion therapy.
However, there is good news. Manufacturers have copay assistance and financial assistance programs to help offset the cost to patients. These programs will often cover up to $20,000 per year per patient and significantly reduce, or remove, any financial burden a patient may face for the drug’s administration.
One thing every patient should ask of a potential infusion center: will you research and enroll patients in copay and financial assistance programs? High-quality infusion centers will do these activities proactively for patients.
Finance & insurance FAQs
What insurance do you take at Local Infusion?
We work with many major insurance companies, including Anthem, Aetna, Cigna, Harvard Pilgrim Healthcare, Human, Medicare, and United Healthcare.
What if you do not take my insurance?
If we are not in-network with your insurance plan we may still be able to bill your insurance carrier out-of-network. If you do not have out-of-network benefits available, we are also able to see you as a Self Pay patient. Feel free to contact our team if you would like more details.
What is copay assistance?
A copay assistance card (also known as a copay savings program, copay coupon, or simply a copay card) is essentially a coupon that makes a medication way more cost-effective for you. You simply sign up for the program (and Local Infusion can also help you out here!) — usually via a form on your drug manufacturer’s website or an independent copay card website — download or get your card in the mail, and show it at the pharmacy when you go to fill your prescription.
Instead of paying a high copay (perhaps $50, $75, or more, depending on the specifics of your insurance coverage), you pay a lot less for infusion services. In some cases, you might not owe anything at all. The pharmaceutical company covers the difference.
Who is eligible for copay assistance?
Program restrictions vary, but generally anyone who has private health insurance (not Medicare or Medicaid) is eligible to enroll in a copay assistance program. You don’t typically have to prove that paying your regular copay for the medication would present a financial hardship.
READ MORE: Why Local Infusion
We caught up with Dr. Paredes to learn more about his work as a gastroenterologist, the biggest misconceptions around Crohn’s disease, and his hopes...
Learn more about Pemgarda, a groundbreaking preventative treatment offering the immunocompromised a new layer of defense against Covid-19.
Insurance, claims, prior authorization, precertification, deductibles….the list of healthcare terms goes on and on (and on). Needless to say, it’s...